Vascular conditions affect the veins and arteries in the body, which conduct oxygen to every living cell. In many cases, vascular conditions can be treated without surgery.
Even so, it’s important to see a vascular surgeon, as these problems can impact other parts of your body. Read more+
Exercise, diet, or medication may be prescribed as a first step in regaining your vascular health. Should surgery be needed, our physicians are experienced in every type of surgical intervention, and successfully perform over 1,000 procedures annually, with excellent results.
Peripheral arterial disease is a common problem, affecting more than 10 million people.
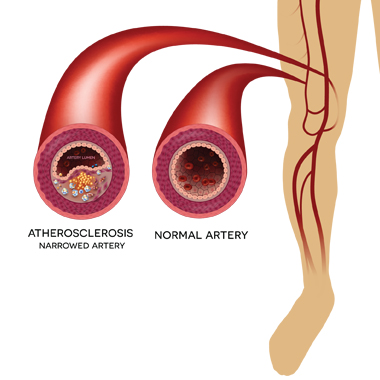
You’ve likely heard of “hardening of the arteries,” which is what peripheral atherosclerosis (PAD) is more commonly called. This is a chronic disease in which plaque gradually builds up in the arteries to the legs. If allowed to progress, blood flow in an artery can become limited or blocked altogether.
While PAD is most common in people who are 65 or older, it can occur at nearly any age. Peripheral atherosclerosisis a warning sign that other arteries, including those in the heart and brain, may also be blocked—increasing the risk of a heart attack or stroke.
The causes of peripheral atherosclerosisis include smoking, high cholesterol or high triglycerides, high blood pressure, diabetes, kidney failure, and obesity.
People with a personal history of vascular disease, heart attack, or stroke have a one in three chance of also having PAD.
African Americans are more than twice as likely to have PAD than their white counterparts. Genetic factors also play a role, but they are not well understood.
Symptoms
At least half the people with PAD do not show any symptoms. Those who do may have pain or aching when walking, climbing stairs or exercising, which is relieved after resting. Other symptoms of PAD include:
- Cramping in the legs, thighs, and calves
- A weak or absent pulse in the legs or feet
- Sores or wounds on toes, feet or legs that heal slowly, poorly, or not at all
- Color changes in skin, paleness, or blueness
- Lower temperature in one leg compared to the other leg
- Poor nail growth and decreased hair growth on toes and legs
An open wound or ulcer on your toes or feet can signal a serious case of peripheral atherosclerosisis. Because ulcers can progress to gangrene, they require immediate medical attention.
The initial diagnostic test for peripheral atherosclerosisis is the ankle brachial index (ABI). The vascular surgeon will take a blood pressure reading at the ankle and compare it to that in the arm.
An angiogram is typically taken to determine where plaque has built up in the arteries and to assess treatment options. Angiograms can be done with a CT or MRI. Sometimes, a catheter-directed angiogram is done, which involves placing a thin tube into the artery and injecting dye to see where the blockages are located.
Peripheral atherosclerosisis is usually treated by aggressively managing the risk factors with lifestyle changes and medication. These include quitting smoking, controlling blood pressure and cholesterol, controlling diabetes and losing weight.
Studies show that exercise will not make PAD worse. In fact, following a regular exercise program can significantly improve the symptoms of PAD for many people.
If the condition is causing serious symptoms, surgical treatments including balloon angioplasty, stent placement, or surgical bypass can be effective in improving the blood flow to the affected leg.
While age, race, medical history and genetic factors cannot be controlled, there are steps you can take to reduce the risk of developing PAD:
- Avoid smoking and tobacco use
- Exercise regularly
- Maintain a healthy weight
- Eat a well-balanced, low sodium, low fat diet
If you have been prescribed medications to control high blood pressure, high cholesterol or triglycerides, diabetes or kidney failure, be sure to continue taking them as recommended.
Overview
Peripheral arterial disease is a common problem, affecting more than 10 million people.
You’ve likely heard of “hardening of the arteries,” which is what peripheral atherosclerosis (PAD) is more commonly called. This is a chronic disease in which plaque gradually builds up in the arteries to the legs. If allowed to progress, blood flow in an artery can become limited or blocked altogether.
While PAD is most common in people who are 65 or older, it can occur at nearly any age. Peripheral atherosclerosisis a warning sign that other arteries, including those in the heart and brain, may also be blocked—increasing the risk of a heart attack or stroke.
Causes / Symptoms
The causes of peripheral atherosclerosisis include smoking, high cholesterol or high triglycerides, high blood pressure, diabetes, kidney failure, and obesity.
People with a personal history of vascular disease, heart attack, or stroke have a one in three chance of also having PAD.
African Americans are more than twice as likely to have PAD than their white counterparts. Genetic factors also play a role, but they are not well understood.
Symptoms
At least half the people with PAD do not show any symptoms. Those who do may have pain or aching when walking, climbing stairs or exercising, which is relieved after resting. Other symptoms of PAD include:
- Cramping in the legs, thighs, and calves
- A weak or absent pulse in the legs or feet
- Sores or wounds on toes, feet or legs that heal slowly, poorly, or not at all
- Color changes in skin, paleness, or blueness
- Lower temperature in one leg compared to the other leg
- Poor nail growth and decreased hair growth on toes and legs
An open wound or ulcer on your toes or feet can signal a serious case of peripheral atherosclerosisis. Because ulcers can progress to gangrene, they require immediate medical attention.
Diagnosis
The initial diagnostic test for peripheral atherosclerosisis is the ankle brachial index (ABI). The vascular surgeon will take a blood pressure reading at the ankle and compare it to that in the arm.
An angiogram is typically taken to determine where plaque has built up in the arteries and to assess treatment options. Angiograms can be done with a CT or MRI. Sometimes, a catheter-directed angiogram is done, which involves placing a thin tube into the artery and injecting dye to see where the blockages are located.
Treatment
Peripheral atherosclerosisis is usually treated by aggressively managing the risk factors with lifestyle changes and medication. These include quitting smoking, controlling blood pressure and cholesterol, controlling diabetes and losing weight.
Studies show that exercise will not make PAD worse. In fact, following a regular exercise program can significantly improve the symptoms of PAD for many people.
If the condition is causing serious symptoms, surgical treatments including balloon angioplasty, stent placement, or surgical bypass can be effective in improving the blood flow to the affected leg.
Reducing Risk
While age, race, medical history and genetic factors cannot be controlled, there are steps you can take to reduce the risk of developing PAD:
- Avoid smoking and tobacco use
- Exercise regularly
- Maintain a healthy weight
- Eat a well-balanced, low sodium, low fat diet
If you have been prescribed medications to control high blood pressure, high cholesterol or triglycerides, diabetes or kidney failure, be sure to continue taking them as recommended.
Consultation
Take the first step to looking and feeling better! Meet our doctors and talk about the procedures available to you.Patient Center
Complete your pre-visit forms, and learn more about insurance coverage and convenient payment options.FAQs
Have questions or concerns about your vein conditions? See the answers to our patients’ most common questions.

